Lukman Ismaila, Fellow, Datasphere Initiative
In this blog post, which is part of my fellowship with the Datasphere Initiative, I further my investigation into the lack of medical imagery data for scientific research in Africa. This blog focuses on ways to improve current health data policies and proposes a Biobank for medical imagery data in African regions.
Introduction
Several regions in Africa face challenges due to low data coverage.¹ For instance, when considering mortality data alone, out of the 46 countries in the region, only four countries (Algeria, Mauritius, Seychelles, and South Africa) exhibit coverage rates of 75% or higher.² Besides the availability of data, quality is also an issue because, while some government management information systems might generate considerable data, that data is rarely used due to concerns about bias, quality, and timeliness.³ These are only a few examples.
For Africa’s health research ecosystem to improve, it is crucial that trustable and quality data is created and made accessible to support impactful scientific discoveries.⁴
Similarly, effective responses to pandemics require high-quality, comprehensive datasets that can inform policymaking and enhance healthcare decision-making.⁵ However, several factors still hold this possibility back, as discussed in my previous post on the State of Medical Data in Africa: A Case of Barriers to Science in Africa.
To make this situation even more complex, various countries in Africa have adopted data privacy and data protection laws. And while those are core elements to inform data management, they can pose various challenges to data sharing in health – a sector that is highly dependable on personal and sensitive data.
Positive activity is, however, noticed at the cross-government level – with the push for a single health information exchange (HIE) policy, accompanied by implementation strategy, technical standards, and security norms.⁶ And also at the practitioner level, with communities focused on improving computer vision skills, knowledge and collaboration, and other cutting-edge techniques for research. These communities include Black in AI (BAI), Deep learning indaba (DLI), Data Science Nigeria (DSN), Ro’ya-CV4Africa, Masakhane, and Sisonke Biotik.
Thus, building on this wave of opportunity and awakening for the positives of data sharing and open science, my focus in this new piece is to suggest a pathway that potentially holds tremendous promise for propelling Africa’s health sector forward. For that, I briefly discuss: the impact of data sharing on health research in Africa and the rise of sustainable pan-African data policies. I then focus the discussion on the issue of medical imagery data and present recommendations for enhancing the sharing of this data. To then support moving the needle further, I then call for the establishment of a multi-sectorally owned biobank framework while applying the three core conceptual elements of the datasphere – data, norms, and people.
The awakening of health data sharing policies in Africa
Data sharing policies, including cross-border, can have a significant influence on health research by improving data coverage and data quality through coordination efforts, and then potentially improving the efficiency of research and impact of investments, in addition to supporting better policy-making in response to crises.
At the practitioner level, while not always easy,⁷⁻⁸ by making data more readily available via clear governance protocols and community norms, researchers can build upon the work of others and avoid duplication of efforts. This could potentially – besides supporting human rights³ – help accelerate the pace of discovery and improve the impact of research on current medical services.
For instance, a South African study on data sharing practices among researchers reveals that while vast amounts of healthcare data are being collected and processed to prevent outbreaks, combat epidemics, improve treatment quality, and reduce costs, due to new legislation on data protection, new data governance frameworks are still needed to support responsible sharing. It discovered that the volume of medical imagery data for research, for instance, is rapidly increasing,⁹ potentially offering new insights into health and illnesses. However, without clear coordination within South African authorities, and responsible data sharing and open science approaches such a positive impact might not be felt.
While various data privacy and protection laws are being adopted across the continent – such as the South African Protection of Personal Information Act (POPIA) and the Nigerian Data Protection Regulation, 2019 (NDPR) – they actually provide an opportunity to clarify how data can be handled, strengthening data protection and placing it as a strand for the overall improvement of data management, while allowing for the flow of data across African regions.⁹ In this context, in order to realize the full potential of eHealth on the continent, there is a push for African nations to develop a single health information exchange (HIE).⁶ In this sense, the African Union’ Africa Centers for Disease Control and Prevention (Africa CDC) – with the support of a multistakeholder experts group – has proposed the creation of a pan-African Union HIE and published a guide on its creation and data policies.¹⁰
Supporting data sharing policies in African countries
There are several steps that could be taken to improve data governance and responsibly unlock the value of data for health research in Africa. Those steps include, for instance:
- Create organizations that can generate reliable, unbiased data: Organizations and agencies that focus on quality and reliable data creation must be encouraged by stakeholders in African regions. This step is necessary because it makes quality data available for health research purposes in Africa. These organizations can work towards developing robust data collection methods, implementing standardized protocols, and ensuring data quality and integrity. By fostering a culture of transparency, accountability, and rigorous data practices, these organizations can provide trustworthy and high-quality data that can serve as a solid foundation for health research, policy-making, and decision-making processes in Africa.
- Increase funding and allocate it differently: Financial support provided in African regions needs to be increased with an additional focus on individual project allocation. Adequate financial resources should be allocated to support data collection, management, analysis, and infrastructure development. This includes investing in modern technologies, data storage systems, and skilled personnel to handle and interpret the data effectively. Additionally, funding should be directed towards capacity-building initiatives to enhance data literacy and analytical skills among researchers and health professionals. By ensuring sufficient funding and strategic allocation, Africa can strengthen its data ecosystem, promote research collaborations, and ultimately drive evidence-based decision-making and advancements in health outcomes across the continent.
- Establish well-articulated data policies and standards: It is important to have clear guidelines and standards in place that outline the expectations and responsibilities of researchers with regard to data sharing. This includes guidelines on issues such as data quality, relevancy and useability, data anonymization, data security, interoperability, and the proper attribution of data sources.
- Develop mechanisms for oversight and accountability: To ensure that data is used in an appropriate and transparent manner, it may be necessary to establish mechanisms for oversight and accountability. This could include the development of a formal system for reviewing and approving data-sharing requests, as well as processes for addressing any concerns or issues that may arise.
- Foster a culture of data sharing: To encourage researchers to share data, it is important to create a culture that values and rewards data sharing. This could include providing training and support to researchers to help them understand the importance of data sharing, as well as recognizing and rewarding researchers who make their data available to others.
- Invest in infrastructure and technology: To facilitate data sharing, it is necessary to invest in infrastructure and technology to support the collection, storage, and analysis of data. This could include investments in data management systems and networks to support the sharing of data across institutions and regions. Health facility assessments can provide data on the availability and quality of health services and the health system resources that are required for their success. Facility assessments are a unique source of statistics on service availability, generating data on facility infrastructure, infection control, services offered, staffing, laboratory facilities, treatments, guidelines, and supplies. Indicators can be calculated to track the percentage of health facilities in a given country or region that offer a specific, measurable treatment or service.
Proposing a Medical Imagery Bio-bank for Africa
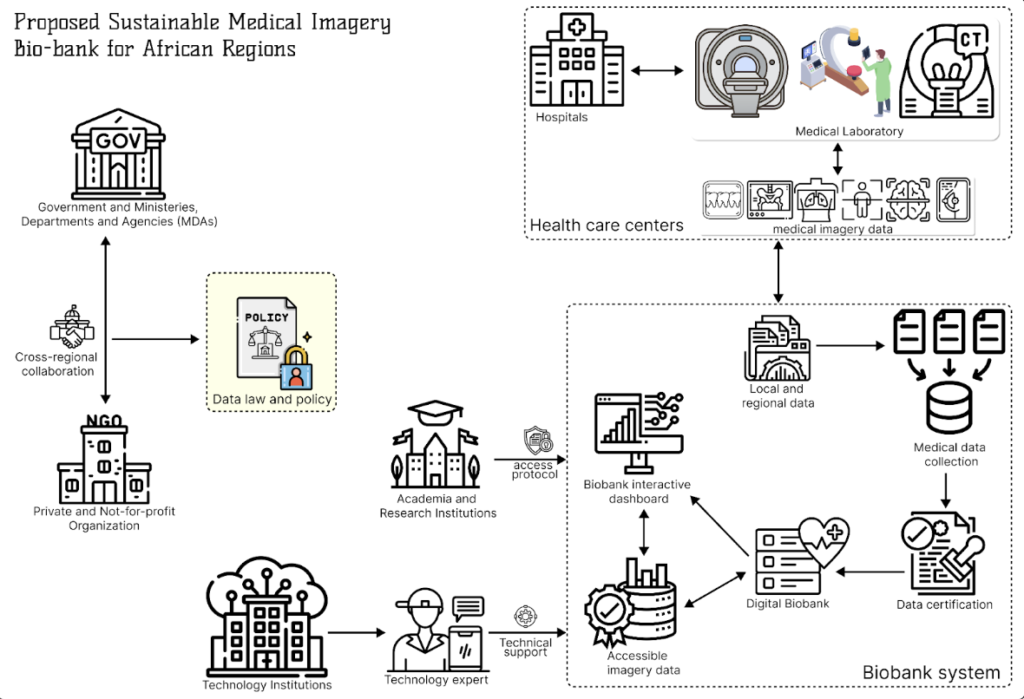
To advance some of the elements enumerated above, I introduce a multi-actor framework for data governance that – while preserving privacy and fostering data protection, allows for collaboration and data sharing in support of health research in Africa: a Biobank of Medical Data, with special focus on imagery data.
Core actors in this framework and their roles include:
- Not-for-profit organizations will play a vital role in the establishment and operation of the medical imagery Biobank by advocating for data sharing and research collaboration, mobilizing resources and funding, and facilitating partnerships.
- The government and Ministries Departments Agencies (MDAs), should be responsible for creating an enabling environment through policy development, funding support, collaboration promotion, and governance establishment.
- Healthcare centers that will contribute medical imagery data, ensuring accuracy, security, and privacy
- Academia and Research institutions, will conduct research, develop policies, and promote ethical data use.
- Technological institutions should provide technical expertise, infrastructure, and innovation for the Biobank’s operation, including secure data storage, interoperability, and data quality control.
This multi-actor framework should then address the issues of medical data availability by ensuring clear and standard processes for i) data creation and collation, ii) data quality certification, iii) data privacy and security, iv) trustable data storage and access protocols, and v) equitable data access and usage rights.
An initial overview of the relationship between these actors follows in the figure below. In my next post, I will further detail the process and how data would then flow within this framework.
Conclusion
The introductory discussions and ideas in this post shed light on the profound influence of data sharing on health research. It also highlights the enthusiasm of active research communities for collaboration, and examines the rise of sustainable pan-African data policies. Our exploration into the realm of data sharing and governance in Africa’s health research landscape points to the need for the creation of multi-actor frameworks that allow for more and better data and data governance based on clear roles and coordination. To support these efforts, I suggest the establishment of a multi-actor biobank where data, norms, and people work hand in hand to drive innovation and improve healthcare outcomes. I believe that – with such collaborative, open, and trust-based frameworks – Africa’s health sector can harness the power of medical data, improving discovery and the continent’s people’s health outcomes.
References
- “Data for African Development,” Center For Global Development | Ideas to Action. https://www.cgdev.org/working-group/data-african-development (accessed Jun. 22, 2023).
- Mbondji, Peter Ebongue, et al. “Health information systems in Africa: descriptive analysis of data sources, information products and health statistics.” Journal of the Royal Society of Medicine 107.1_suppl (2014): 34-45.
- Knoppers, Bartha M., et al. “A human rights approach to an international code of conduct for genomic and clinical data sharing.” Human Genetics 133 (2014): 895-903.
- Lilja, Erika. “Threat of policy alienation: Exploring the implementation of Open Science policy in research practice.” Science and Public Policy 47.6 (2020): 803-817.
- Brand, Dirk, et al. “Data sharing governance in sub-Saharan Africa during public health emergencies: Gaps and guidance.” South African Journal of Science 118.11-12 (2022): 1-6.
- Mamuye, Adane L., et al. “Health Information Exchange Policy and Standards for Digital Health Systems in Africa: A Systematic Review.” PLOS Digital Health, vol. 1, no. 10, Oct. 2022, p. e0000118. PLoS Journals, https://doi.org/10.1371/journal.pdig.0000118.
- Hardwicke, Tom E., et al. “Data availability, reusability, and analytic reproducibility: Evaluating the impact of a mandatory open data policy at the journal Cognition.” Royal Society open science 5.8 (2018): 180448.
- Bijak, Jakub, et al. “Open Science, Replicability, and Transparency in Modelling.” Towards Bayesian Model-Based Demography: Agency, Complexity, and Uncertainty in Migration Studies (2022): 175-183.
- Staunton, Ciara, et al. “Data Protection, Data Management, and Data Sharing: Stakeholder Perspectives on the Protection of Personal Health Information in South Africa.” PloS One, vol. 16, no. 12, 2021, p. e0260341. PubMed, https://doi.org/10.1371/journal.pone.0260341.
- National Information Technology Development Agency, “Nigeria Data Protection Regulation (NDPR): Implementation Framework” Nov 2020
- “African Union Health Information Exchange Guidelines and Standards,” Africa CDC. https://africacdc.org/download/african-union-health-information-exchange-guidelines-and-standards/ (accessed Jun. 22, 2023).